
HHPs and Women Health

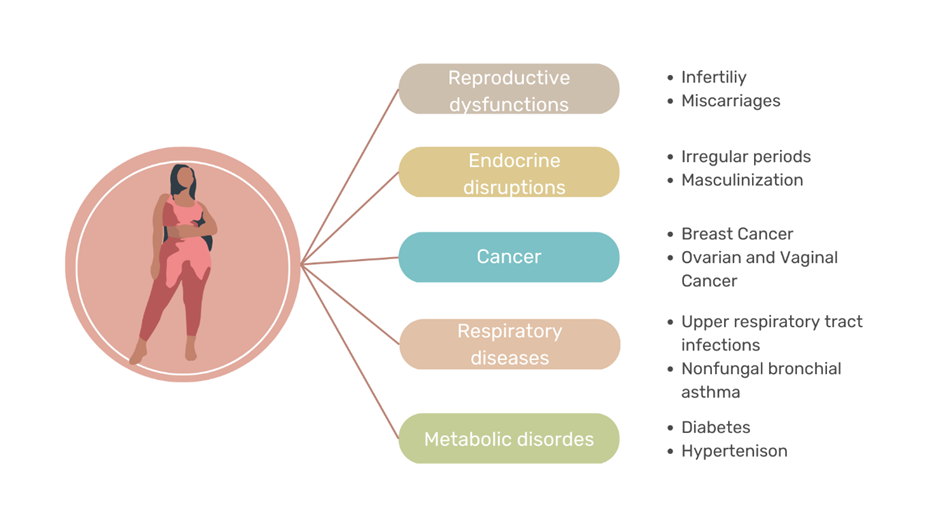
Women make up a significant proportion of the agricultural workforce (43%), yet they are often overlooked when it comes to pesticide exposure risks. Because it was often believed that women do not engage in farming practises as a profession, there were very few studies on women farmers. However, it is to note that, Women are more likely to be exposed to pesticides because they often work on small farms that lack the necessary protective gear. Moreover, women’s clothing does not typically have enough coverage to protect them from chemical exposure. Exposure can lead to various health problems, including reproductive health problems, cancer, and endocrine disruption. The accumulation of pesticides in the body over time can have chronic health implications for women that can lead to long-term disabilities and death. Since women play a primary role in pregnancy and childbirth, such exposure to hazardous chemicals tends to have a direct impact on children born to them. Children born to women exposed to pesticides during pregnancy have a higher risk of birth defects, mental retardation, and various other health complications.
HHPs and Hormone disruption

Women have higher levels of fat tissues compared to men ( 15% essential fat Vs. 3 % essential fat). They also have higher level of hormone-sensitive tissues and are primarily involved in child-carrying and rearing. This makes them more vulnerable to the toxic effects of Highly Hazardous Pesticides. These hazardous chemicals are known to disrupt the endocrine system, which regulates hormones involved in reproduction, growth and metabolism. Endocrine disruptors (in this case, HHPs) typically bind tightly to androgenic and estrogenic receptors in humans and mimic their actions (act as an agonist), causing hyperactivity, or they can serve as antagonists, causing opposite reaction. They may also obstruct a hormone’s organic biochemical production. For instance, HHPs like Mancozeb, ziram, zineb, etc. interfere with thyroid production. Offsprings may experience a variety of neurological, behavioural, and reproductive abnormalities as a result of the endocrine disruption in the mother
HHPs and Cancer
Cancer is yet another serious health effect of pesticides on women. Studies have linked pesticide use to a highly increased risk of developing cancer in women. Breast cancer is the leading type of cancer among women. In PANAP study, titled, ‘Pesticides and Breast cancer, a wake up call’, 98 pesticides from around the world was found to be linked with breast cancer. Most of these pesticides were also found as residues in breast milk. The findings of the study from women farmers in Jaipur, India indicated that, regardless of their age, nutrition, or geographic location, breast cancer patients were found to have significantly greater levels of organochlorine pesticide residues than healthy females (Mathur. V et al, 2002). Other than breast cancer, there is also an elevated risk of lung cancer among women farmers. Many systematic reviews discovered an overabundance of proof suggesting that pesticide exposure and the risks of several different cancers, including brain, prostate, and kidney cancers, as well as NHL and leukaemia, are positively correlated in woman farmer.

HHPs and Reproductive Health

HHPs also have a high-end effect on fertility and reproductive functions in women. These chemicals can affect the development of the reproductive system in women, leading to fertility problems and pregnancy-related complications. These chemicals have been linked to reproductive issues such as decrease in female hormone, endometriosis, irregular menstruation and infertility. A Study which has noted down precocious puberty in a 4-month-old girl marked with increased breast size, uterine length and 3 sets of the menstrual cycle due to parental exposure to multiple pesticides (Gaspari et al, 2011) demonstrates the impacts of pesticide on women and subsequent generations. There is also an increased percentage of abortion and stillbirths in women who are exposed to pesticides noted from cotton farms in India (Rupa et al,1990).
The socio-cultural environment also plays a role in determining pesticide exposure risks for women. Women’s lack of awareness on the subject makes it difficult for them to comprehend the implications of pesticide exposure. Culturally, women are hesitant to speak up for their rights in rural households and are reluctant to disclose their symptoms in the perception that they may be perceived as weak or undermine their femininity. Women may also be reluctant to practice safe agriculture methods as they fear it may forfeit their income source for unwanted expenses, leading to chronic exposure. With the alarming rate of unsafe practices, health risks posed by pesticide exposure are inclined to only grow. Creating a safe workplace is the first step in helping female workers avoid the negative impacts of pesticides. Some of the things we can do to advocate safety for our women farmers encompass assessments of risk, better medical support, the development of good package of practises (POPs) and standard operating procedures (SOPs), as well as programmes that ensure and provide maximum safety, raise awareness and boost their sense of empowerment. Healthy homes are essential, as are healthy women farmers.
References
Gaspari, L., Paris, F., Jeandel, C., & Sultan, C. (2011). Peripheral precocious puberty in a 4-month-old girl: role of pesticides? Gynecological Endocrinology, 27(9), 721-724.
Mathur, V., Bhatnagar, P., Sharma, R. G., Acharya, V., & Sexana, R. (2002). Breast cancer incidence and exposure to pesticides among women originating from Jaipur. Environment international, 28(5), 331-336.
Meriel, W. (2007). Pesticides and Breast cancer. A Wake up call.
Rupa, D. S., Reddy, P. P., & Reddi, O. S. (1991). Reproductive performance in the population exposed to pesticides in cotton fields in India. Environmental Research, 55(2), 123-128.
