b
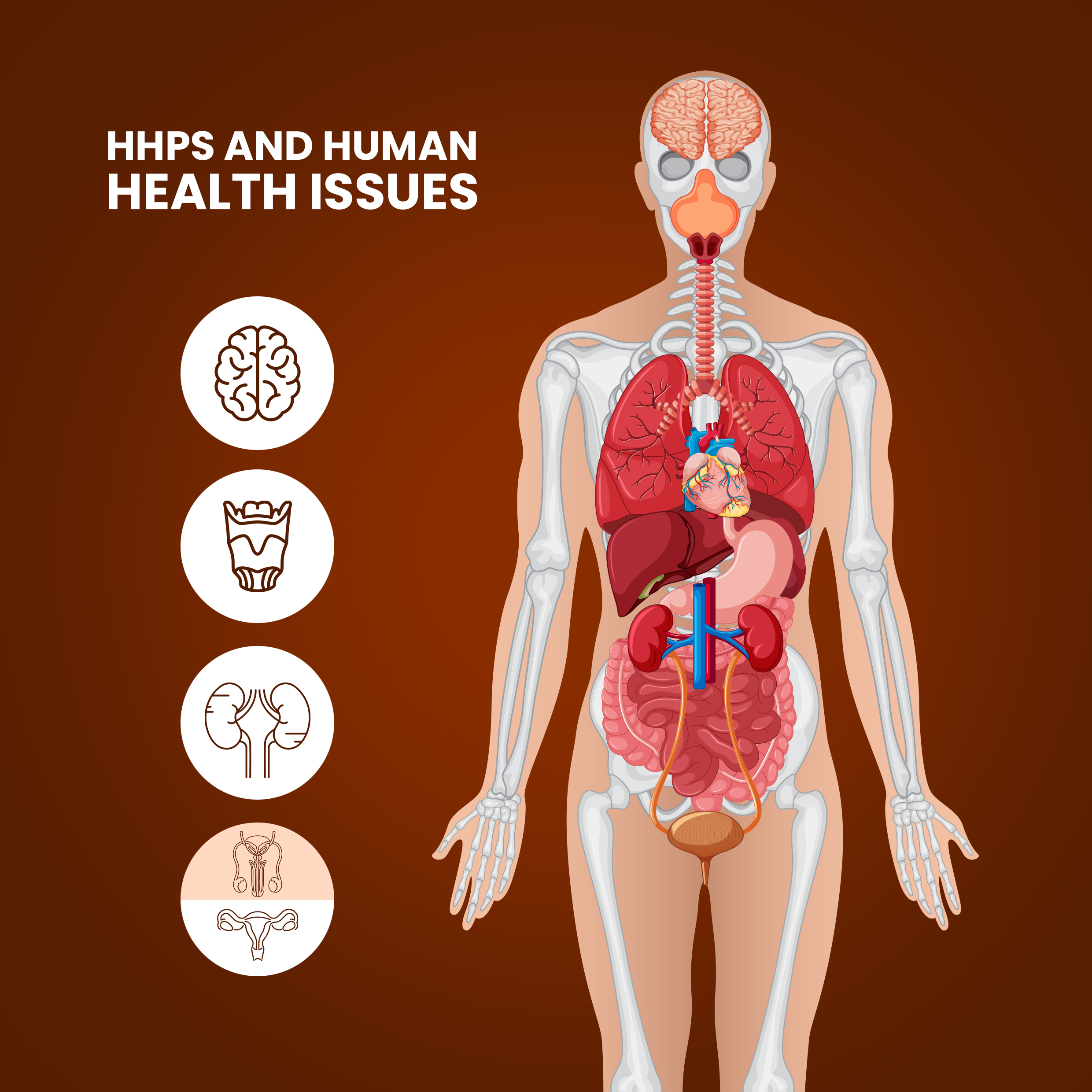
HHPs AND HUMAN HEALTH ISSUES
s
The harmful effects of pesticides in our food chain have already been proven to be a health hazard. Highly Hazardous Pesticides affect health the most, where they cause acute and delayed health effects in people who are exposed. The vast number of pesticides in our food contribute to poor health. Most of these pesticides, can cause contact dermatitis and can enter the body through any route of transmission. They can bind with other functional molecules in the body, can be absorbed into the blood and lymphatic system, can lodge in organs, can act as hormone analogues and can even induce mutations. This, in turn, can lead to a wide array of diseases. Long term exposure to pesticides increases risk, by many folds and increases the chance of confronting multiple disorders and system failures. Changes induced in germ cells and other reproductive cells, can affect the next generation and thereby, become a heritable change. Reduced immunity, loss of motion coordination and reproductive fitness are the most common side effects of pesticide use. Cancer is one of the most studied effects of pesticide use. Endocrine disruption, can lead to altered biological hormone function and thereby affect homeostasis. HHPs can also cause acute and chronic health effects, such as carcinogenicity, reproductive and developmental toxicity, neurotoxicity, and endocrine disruption.
HHPs in India can cause…..

21 of the HHPs cause cholinesterase inhibition

33 pesticides are suspected of having endocrine disruption effects.

20 HHPs are reproductive toxicant.
26 HHPs have carcinogenic potential
1 HHP is mutagenic
How HHPs enter into our body?

We know many of these individual pesticides are a cause for concern. Pesticides can easily transfer from the farm to the home through various ways, such as contaminated soil or drift. Generally, pesticides are absorbed through skin, oral or inhalation routes, yet because of leeching, mobility and bioaccumulation potential, they reach into ground water and surface water. This is a problem for many people living in the area without safe drinking water. Moreover, pesticide residues in food and drinking water can lead to long term exposure and health risks.
Human exposure to pesticides may occur through occupational exposure in agricultural workers who mix, load, transport, and apply formulated pesticides. Workers’ general hygiene practices during pesticide usage can significantly affect exposure. In some circumstances, exposure to pesticides might result from unintentional chemical spills, leaks, or defective spraying equipment. Liquid pesticides can spill, while solid particles can form dust while application.
HHPs and Acute Toxicity
bb
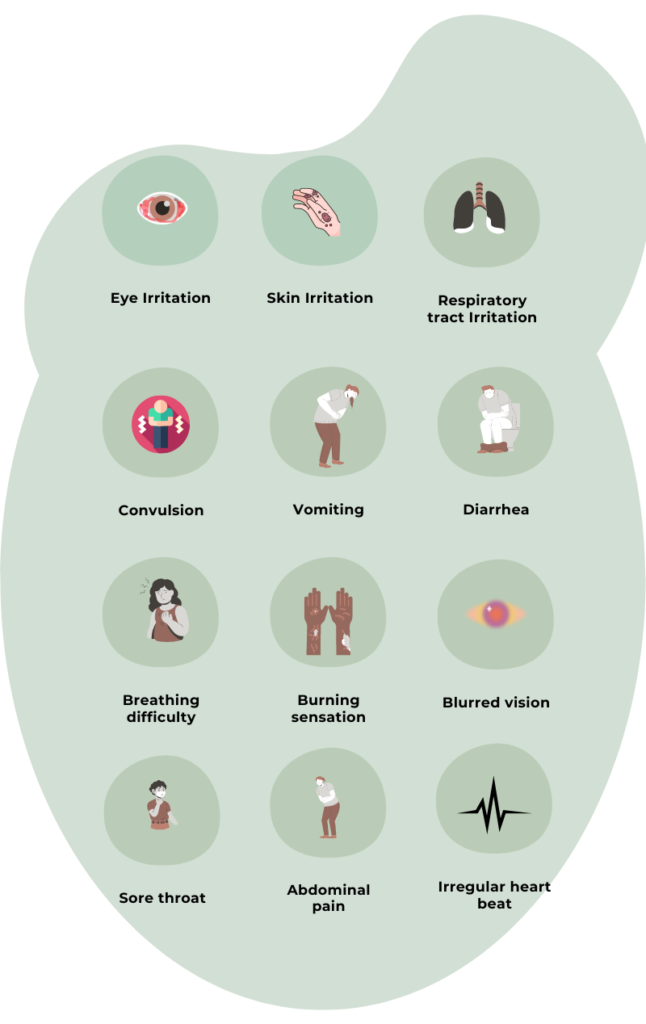
The effects of a single dose or repeated exposure over a brief period of time are referred to as acute toxicity of a pesticide.They refer to the immediate range of health consequences brought on by pesticide exposure. The four possible exposure pathways are cutaneous (skin), inhalative (lungs), oral (mouth), and visual (eyes). Acute toxicity based on the LD50 is denoted by signal words like Poison, Danger, Warning, and Caution. HHPs can cause acute toxicity or immediate toxicity upon a single exposure. The common symptoms include increased sweating, salivation, tears, and respiratory secretions, as well as headaches, nausea, and dizziness, twitching, weakness, tremor, incoordination, vomiting, abdominal cramps and diarrhoea.
When pesticides are prepared, mixed, decanted, and applied, unintentional pesticide poisoning occurs. Annually, there are around 385 million instances of UAPP worldwide, with 11,000 fatalities. According to Boedkar et al (2020) studies on Unintentional poisonings around the world, 66,000 farmers are poisoned in India every year. The most frequent type of intentional poisoning is self-poisoning. In India, HHPs form the major share of pesticides used for intentional poisoning due to their severe toxicity and cheap availability. According to the 2021 National Crimes Record Bureau (NCRB) Accidental Deaths and Suicides in India report, 7950 pesticide-related mishaps happened in India in 2021.
WHO Classification by Hazard
Based on the acute toxicity of the technical active substance, the WHO classification of pesticides by hazard, is utilised to differentiate between the more and the less hazardous forms of specific pesticides. Acute oral and dermal toxicities in rats serve as the foundation for an active ingredient toxicological profile. Three of the HHPs registered in India are extremely hazardous or belong to WHO class 1a. 11 HHPs in India are highly dangerous or belongs to class 1 b. 23 HHPs are in the H330 subclass (inhalation toxicity) and 11 HHPs are in WHO class 1b or are highly dangerous. 55 Highly Hazardous Pesticides belong to class 2 or moderately Hazardous category, and 21 HHPS belong to class 3 or are slightly hazardous. The H330 subclass of pesticides (inhalation toxicity) also includes 23 HHPs registered in India.
HHPs and Chronic Health Issues
cc
HHPs and Cancer
Numerous studies have connected pesticide exposure to an elevated risk of several cancers, including leukaemia, lymphoma, and brain cancer in farmers. Farmers are more vulnerable to pesticides than the general populace due to various access points and contact with higher concentrations of pesticides. Farmers who use pesticides have been discovered to have 45 different types of cancer. There is no doubt that pesticides, particularly HHPs, are partially accountable for the increasing incidence of cancer. These HHPs interfere with important biochemical pathways involved in cell control and cause cancer. Furthermore, multiple studies have demonstrated that people who work in agriculture or who reside close to agricultural areas, where pesticides are widely used are more likely to develop cancer than those who do not. An elevated risk of non-Hodgkin lymphoma (NHL) of 80% was discovered in a population-based study conducted in Washington State (US) among those who reported using DDT and Organophosphorous pesticides are found to increase the chance of colorectal cancer (Abolhassani, M et al, 2019) in farmers.
Children of farmers and applicators also face the worst case. The negative impacts of pesticide use also affect the children of pesticide applicators. A US-based study (Buckley et al., 2000) found that children of parents who were exposed to pesticides and who continued to use them throughout their infancy had an increased risk of developing acute myeloid leukaemia. Other types of cancer are also highly prevalent among children of pesticide applicators.

HHPs and Reproductive Toxicity
The risk of sperm abnormalities, poor fertility, a lack of male offspring, spontaneous abortion, birth malformations, or foetal growth retardation may increase if men or women are exposed to specific pesticides at adequate levels (Linda M. Frazier, 2007). According to studies, working in agriculture increases the likelihood of developing certain morphological sperm abnormalities, such as a lower sperm count per ejaculate and a decreased proportion of viable sperm. Similarly, cases of infertility among women and significant risk of reproductive disorders in women employed during pregnancy in conditions of pesticide exposure was noted in multiple studies. In comparison to women who never used pesticides, Women who used pesticides experienced longer menstrual cycles and increased odds of missed periods. Furthermore, in comparison with women who had never used pesticides, women who had used possibly hormonally active pesticides had a 60–100% higher chance of having long cycles, missed periods, and intermenstrual haemorrhage (Farr. S.L et al, 2004). In India, 20 HHPs registered are known to cause reproductive toxicity.
HHPs and Endocrine Disruption
Normal growth and development, metabolism, reproduction and newborn development depend on balanced hormone levels and functions. Small lipophilic molecules known as endocrine disruptors imitate, inhibit, or reduce the activity of hormones by interacting with several endocrine system components. By altering hormone synthesis patterns, stimulating hormone function or blocking it by occupying the receptor site, pesticides can act as endocrine-disrupting chemicals that affect the reproductive balance in humans. There are 33 identified HHPs in India that cause endocrine disruption. The functioning of the thyroid, the central nervous system, metabolic function, and the body development are all impacted by endocrine disruption along with reproductive dysfunctions as all are hormone-mediated. Precocious puberty, polycystic ovary syndrome, and early ovarian failure are female reproductive system abnormalities that may be linked to EDC (Costa et al., 2014). In addition, exposure to EDs can lead to increased endometrial growth, uterine fibroids, irregular menstruation, infertility, a higher risk of breast cancer, and vaginal cancer. EDs are linked to the higher prevalence of prostate cancer in male humans exposed to pesticides (Settimi et al., 2003).

HHPs and Neurotoxicity
The nervous system is the primary target in insects for the major portion of insecticides, therefore the majority of insecticides frequently have neurotoxic consequences in people (Costa, L et al., 2008). More frequent insecticide users among pesticide applicator subjects were more likely to develop neurological symptoms. Numerous studies have linked increased pesticide use to conditions like Parkinson’s, dementia, and Alzheimer’s. In India, 21 of the 120 HHPs had choline-esterase inhibition activity, which results in neurotoxic consequences.

HHPs and Genotoxicity
Certain pesticides cause genetic alteration, which can significantly modify cell function. These pesticides alter the chromosome number, its structure or create Micronuclei fragments. Carcinogenicity and reproductive toxicology may be primarily caused by genotoxicity. All the 210 male employees in Punjab who were exposed to pesticides in an investigative research study showed significant DNA damage (Kaur R et al., 2011). Carbendazim, an HHP registered in India, exhibit mutagenic effect.
References
Abolhassani, M., Asadikaram, G., Paydar, P., Fallah, H., Aghaee-Afshar, M., Moazed, V., … & Moradi, A. (2019). Organochlorine and organophosphorous pesticides may induce colorectal cancer; A case-control study. Ecotoxicology and environmental safety, 178, 168-177
Boedeker, W., Watts, M., Clausing, P., & Marquez, E. (2020). The global distribution of acute unintentional pesticide poisoning: estimations based on a systematic review. BMC public health, 20(1), 1-19.
Buckley, J. D., Meadows, A. T., Kadin, M. E., Le Beau, M. M., Siegel, S., & Robison, L. L. (2000). Pesticide exposures in children with non‐Hodgkin lymphoma. Cancer: Interdisciplinary International Journal of the American Cancer Society, 89(11), 2315-2321.
Costa, E. M. F., Spritzer, P. M., Hohl, A., & Bachega, T. A. (2014). Effects of endocrine disruptors in the development of the female reproductive tract. Arquivos Brasileiros de Endocrinologia & Metabologia, 58, 153-161.
Costa, L. G., Giordano, G., Guizzetti, M., & Vitalone, A. (2008). Neurotoxicity of pesticides: a brief review. Front Biosci, 13(4), 1240-1249.
Damalas CA and Eleftherohorinos IG. Pesticide exposure, safety issues, and risk assessment indicators. Int J Environ Res Public Health. 2011 May;8(5):1402-19. doi: 10.3390/ijerph8051402. Epub 2011 May 6. PMID: 21655127; PMCID: PMC3108117.
Farr, S. L., Cooper, G. S., Cai, J., Savitz, D. A., & Sandler, D. P. (2004). Pesticide use and menstrual cycle characteristics among premenopausal women in the Agricultural Health Study. American journal of epidemiology, 160(12), 1194-1204.
Kaur, R., Kaur, S., & Lata, M. (2011). Evaluation of DNA damage in agricultural workers exposed to pesticides using single cell gel electrophoresis (comet) assay. Indian journal of human genetics, 17(3), 179.
Settimi, L., Masina, A., Andrion, A., & Axelson, O. (2003). Prostate cancer and exposure to pesticides in agricultural settings. International journal of cancer, 104(4), 458-461.
